Co Author: Dr. Swati Mahajan
5 mins read
As per the Investment Opportunities in India’s Healthcare Sector Report (NITI Aayog, 2021) the healthcare sector in India grew with a Compound Annual Growth Rate (CAGR) of 22% since 2016, employing 4.7 million people. Currently, healthcare in India is either public funded, aided by non-profit partners, or undertaken through private initiatives such as Corporate Social Responsibility (CSR) grants, philanthropy grants, and High Net worth Individual (HNI) donations. Now, with the National Health Policy (NHP), 2017, codifying and specifically referring to leveraging the potential of private sector engagement in primary health care (Policy objective 2.3.1), Public Private Partnerships (PPP) in healthcare have greater institutional support.
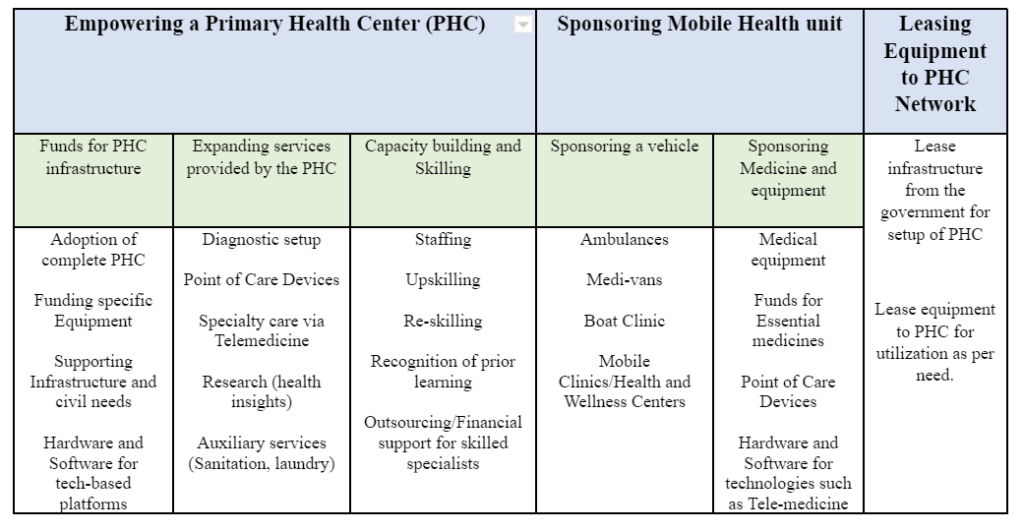
The guiding principle is to make health more approachable and accessible to beneficiaries. Investment opportunities include approaches such as contracting of services, franchising/adopting a hospital, joint ventures, community-based insurance amongst others. Shared below are 3 models for corporates and philanthropic funders looking to support Indian healthcare at the grass-roots level:
Empowering a PHC: Under this approach a corporate partner can support in setting up a functional and efficient Primary Health Centre (PHC)/Health and Wellness Center (HWC). Here, either a PHC/HWC is adopted and developed in collaboration with the state government or an existing PHC is upgraded with infrastructure, equipment, and skilled manpower. The return on investment can be measured in terms of revenue (fee per patient collected), brand visibility (under formal adoption of PHC), public welfare and goodwill (number of patients served, improvement in service delivery metrics). The key idea here is to build these PHCs as “Centers of Excellence” i.e., models for replication and scaling through future initiatives.
Due to the flexible nature of the implementation unit, the scale of investment may vary from complete adoption of PHC to providing specific support such as ensuring availability of diagnostic services, point of care devices, training of staff in the PHC etc. as elaborated in the table above
For instance, in Meghalaya, the NISHTHA initiative by Jhpiego, supported the states by partnering with the private sector for ensuring supply of oxygen concentrators during the pandemic. Similarly, the National Health Mission, has signed an MOU with Krsnna diagnostics in PPP mode to strengthen diagnostic tests. The intervention has resulted in a total of 52 tests being conducted24X7at the PHC/HWC level itself. This was a marked increase from an earlier level of 8-9 tests, available only during specific hours. The project reflects the success of the network governance approach i.e., intersection of state, private and civil society sectors.
The same can also be done for specialized aspects of the PHC. Under the Bio Medical Equipment Maintenance & Management Program (BEMS) program, 29,115 health facilities under the project have been working with private partners to ensure an 80% equipment uptime in Primary Health Centers. In Tripura, Medicity Healthcare Pvt. Ltd. was onboarded in November 2016. This has resulted in 9,460 pieces of equipment being maintained and tracked in real-time, with data available on https://tripura.bmmp.in/spa#/dashboard. The project thus shows the remarkable potential for optimization and skill-based service models within the Indian healthcare space.
Care on the go: mobile care unit approach: Often PHC’s face viability issues, either due to topography of the region or due to low population density, Mobile Care Units (MCU) can help mitigate the difficulty, bringing health services to remote and hilly areas.
In Assam, Centre for North East Studies and Policy Research (C-NES) has been operating 15 Boat Clinics in 13 riverine districts since 2008. Under a PPP arrangement with the National Health Mission, these floating clinics have been treating about 20,000 patients every month (about 240 000 every year).
To further reduce operational challenges, the MCU can be staffed and supported by the local PHC with manpower and medicines. The services availed can be remunerated either through a voluntary community fee at a predetermined price or cross registration with AB-PMJAY.
Further, telemedicine technology can also be used to link patients and the PHC to specialized consultations. The Telemedicine Network Project in the state of Karnataka is one such success story. Introduced in 2001, a technical partnership between Narayana Hrudayalya Bangalore and Indian Space Research Organization, Narayana Hospital is now seeing over 300 patients every day. With health insights through the platform which runs on Azure, SQL Server and Power BI, the model is not only leveraging data for optimization but is also helping patients save close to 81% “out of pocket expenditures” which is otherwise spent on travel and treatment.
Leasing Equipment to PHC Network: A novel approach, leasing can work in two ways:
- Government offers the use of its facilities to private organizations.
- Private organizations lease/ donate equipment/space to the government.
The first model is quite prevalent, where a private partner leases a government facility and offers services on behalf of the government. The remuneration model is thus similar to adopting a PHC approach as discussed above. In the second model, private organizations, in partnership with state government and non-profit partners, can lease out medical equipment to the PHC network, based on the requirements of the center. The equipment may be subject to regular audits for ensuring proper utilization and in case of underutilization, may be transferred to other PHC by mutual agreement. In this approach, the cost of the equipment, may be compensated by a philanthropic partner with a moderate return on investment. A few successful models include initiatives undertaken during COVID-19 relief in the state of Uttar Pradesh and Jharkhand such as deployment of a vaccine storage refrigerator and equipping a MCU.
The Indian healthcare system today has the ideal conditions for public-private partnerships: demand for services, institutional support for the government and ability to scale and create measurable impact. For public sector, corporates, intermediaries and philanthropies, the key question is how they leverage the grassroot investment models, where linking responsible capital with intended beneficiaries.